Headache or Facial Pains
Use these links to learn more about different aspects of headache or facial pains:
Headaches Are a National Dilemma
Over 40% of the U.S. population have suffered from severe headaches at some point in their lives (Zeiger et al, 1977). Over 550 million work days each year are lost because of headaches (Sternbacks, 1986). In 1981, Lance and Drummond reported that in 1200 headache patients, migraines vs. muscle tension type, one could not be distinguished from the other.
Until recently, treatments for headache sufferers has been confined to various methods with marginal success. Pharmacologic, biofeedback, and physiological approaches have helped a number of individuals, but a number of individuals were not significantly improved or they preferred to avoid long term drug, biofeedback or psychologic care. Our main goal is to find and correct the cause of the problem, not to suppress or cover-up the symptoms with drugs or unnecessary surgery.
New Research
New research (Lynn, et al, 1991) has uncovered more of the mysteries of the causes or sources of headaches. The way muscles and bones move above the shoulders differs significantly from the other extremities in many respects. This is an area where right and left nerves, muscles, and vessels must work together. This is essential because the right and left tissue systems are affecting movements of single bones, in essence the mandible (lower jaw) and the cranium (skull). The result of restoring normal physiologic parameters to unbalanced systems was sustained pain relief.
Medical or Biochemical Aspects
When these synergistic or balanced antagonistic tissue systems are unbalanced (asymmetrical motor neuropathic dysfunction), then the right and left components or the elevator or depressor components become dominant. This results in muscle hypertonicity (spasm) at rest or ineffective performance during function. The end product of constant resting muscle hyperactivity (spasm) is decreased blood flow through regional vascular beds (vascular instability). This causes a change in the metabolic path for the production of energy from aerobic metabolism to anaerobic metabolism. The end product of anaerobic metabolism is lactic acid, which is a spasmodic itself and a localized tissue irritant thus causing more spasm and pain, The neurovasomuscular system of the head and neck develop, through life, into functional (efficient) or dysfunctional (inefficient) patterns, much like a person learning to swing a golf club correctly or incorrectly. There is no genetic predetermined pattern of function or dysfunction. The neuromuscular pattern of function or rest, modulated through the reticular activating system is one the body has adapted to either with or without symptoms (pain or headaches). In the symptomatic individuals, the body's adaptive mechanisms have fallen behind the pathophysiologic dysfunctional patterns. The metabolic changes are subtle, but the pain produced is significant.
Headache Relief Is Available
Today, new computerized technology affords specially trained professionals the ability to discover and determine the extent and location of abnormal neurovasomuscular patterns. In many conditions, a computer designed orthosis is necessary to retrain the compromised (neurovasomuscular) tissues. This orthosis promotes tissue healing in much the same way as a cast allows a broken bone to heal. Constant stabilization of dysfunctional tissue systems results in restoring them to functional patterns. The metabolic abnormalities are eliminated and therefore the pain is relieved. Once these tissue systems are restored to normal functional patterns, there are several options available to the patient to maintain long term stability and pain relief.
This physiologic-based treatment has allowed at least 80% pain relief in 95% of the patients treated. The opportunity to experience life without headaches is the result of new computerized technology and new treatment techniques.
What Causes MPD?
We do not think of a person "catching" a heart attach or cancer overnight. Similarly, most people do not "catch" MPD. As a chronic degenerative disease it often takes years to develop. Since we will not find a simple virus, we must consider many different contributing factors.
Have you ever seen a jaw come walking into a dentist's office by itself? We hope not! That jaw happens to be attached to a whole person with a unique personality. This is why we must consider many different aspects of the individual when discussing the cause. We will divide these aspects into three groups: structural, emotional, and biochemical. All of these components are disturbed to some extent when a person suffers from MPD.
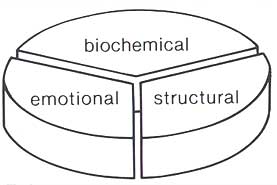
Components of MPD
When diagnosing MPD, we will try to assess the relative impact of each of these components. This will help to determine the most effective course of treatment for you.
It may be that you were not aware of any symptoms until you woke up one day with, for example, an excruciating headache. To explain this, June Biermann and Barbara Toohey in their book, Women's Holistic Headache Relief Book, developed their Dam Theory for those "damn headaches."
They compare headaches to a dam, behind which there is a reservoir. Rain, hail, sleet, snow, and various runoffs all cause the water level behind the dam to rise. When too many of these factors combine, the water spills over the dam, causing a devastating flood in the valley below.
Similarly, many different lifestyle factors can combine which could aggravate MPD - such as structural imbalances, stress, fatigue, certain foods and drinks and even chewing gum. Any one of these is a single drop in the bucket, but taken together, they precipitate into a full-blown MPD condition.
Structural
There is always an underlying structural weakness behind MPD. Nearly all of us have a structural weak spot somewhere in our bodies. For some people, it is their stomach, and they are prone to ulcers. For others, it is their heart, and they are prone to heart attacks. For you, it is your jaw, and this is why you are prone to MPD.
Your structural weakness stems from a condition which dentists call "mal-occlusion" (literally: "bad bite"). This means that your upper and lower teeth do not close together in the right way. Just as a table needs four legs firmly on the floor for support, your teeth must fit firmly together to support the muscles in your face for chewing and swallowing.
Your teeth are part of your skeletal system. They are attached to your jawbone, or mandible, which is one of the 206 bones in your body. The mandible looks something like this:
You can see that your jaw is attached to your head, or temporal bone, by your temporomandibular joints. These two joints happen to be the most complex in your entire body. They are ball and socket joints which have the unique capability of moving in three directions simultaneously - up or down, forward or backward, and to the left or right.
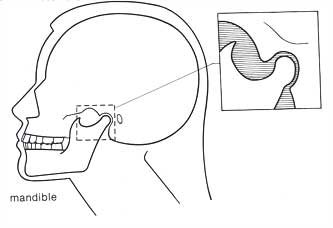
It is important to realize that both your temporomandibular joints and teeth are part of the same bone. The position of your temporomandibular joints is determined by the way in which your upper and lower teeth close together. When your upper and lower teeth are closed together, they are in occlusion. Your occlusion dictates the position of your jaw in relation to your skull. Dentists call this the craniomandibular relationship.
Malocclusion is when your bite is such that your skeletal system is in disharmony with your neuromuscular system. This means that your teeth are forcing the muscles of your face and jaw into a strained and unnatural position.
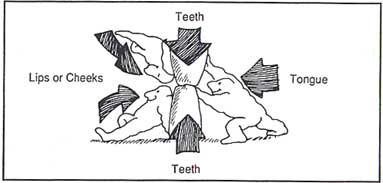
The muscle activity of your face and jaw is extremely complex. Think about it - simultaneously muscles move your lips, tongue, cheeks, eyes, throat, the inner portions of your ear, and your jaw.
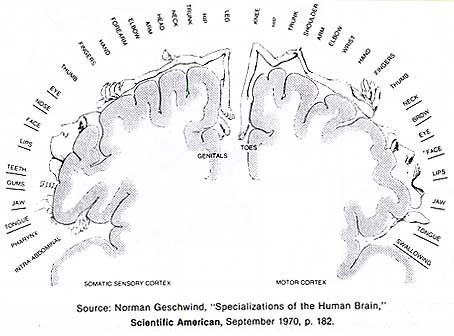
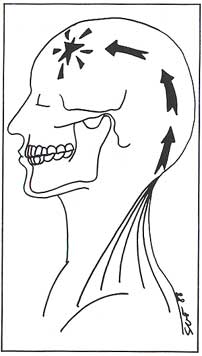
In fact, neurologists have recently mapped out which regions of your brain control the various parts of your body. This diagram shows the control relationship between the cerebral cortex and specific parts of the body:
Distortions occur because the amount of cerebral activity dedicated to a part of the body is not proportional to the size of that part, but to the precision with which it must be controlled. Notice how much of your cerebral cortex is dedicated to your face and neck. You see that the muscle activity in this area is indeed complex.
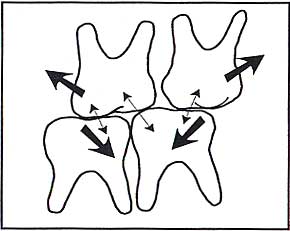
Imbalanced Chewing Forces
Malocclusion, or a "bad bite," can be caused by something extreme, such as a whiplash injury or a blow to the head. But even minor changes, such as a missing tooth or a high filling, can result in MPD.
You probably never connected a missing tooth with your headaches. Most people don't, which is why most MPD headaches are so puzzling. Yet, if your teeth are not providing the proper bracing support for your jaw against your skull, the muscles of your face and jaw compensate by forcing your teeth to come together for chewing and swallowing. Since you swallow at least once each minute, this means your teeth close together over 1,000 times each day and night. When the jaw must twist, or torque, in order for the teeth to close together, the muscles are put into a strained and unnatural position. This muscle spasm is the key to myofascial pain.
Imagine if you had to sit on a chair which had a nail poking out one side of it. Since you would not want to sit on the nail (and probably prefer not to sit on the chair), you would torque your body to one side and hold up one hip.
After a while, this position would become extremely uncomfortable and certain parts of your body would start to feel pretty sore. This is the same thing that happens to the muscles of your face when they are forced into an unnatural position because of your bite. Eventually the strained muscles become sore and painful.
Balance of Forces
Not only do the muscles of your face and jaw become sore because of this constant strain, but they also shorten. This can cause problems in the muscles of your neck, head, back and even down into your chest.
Your head sits delicately balanced on top of your neck because of a complex coordination of these muscles. Imagine it as a baseball balanced on top of a pencil and held in place by a number of rubber bands. Now imagine shortening just one of those rubber bands; some would stretch, some would shorten, and the baseball would be thrown off kilter! Similarly, when even a single jaw, neck or shoulder muscle becomes shortened, all of the other muscles are forced to overwork to keep the head balanced on top of the spinal column.
Muscles which are under constant strain can develop "trigger points." These feel like knots, or nodules, which are painful when you press on them.
Referred Pain
Sometimes trigger points can be the source of referred pain. Referred pain is when a pain originates in a part of the body that differs from the area where it is felt. These can be tricky to detect, because the painful area is not the source of the problem. We are able to detect the real source of pain by mapping the referred pain patterns.
Summary
You see that people who suffer from MPD have a structural imbalance in their jaw-to-skull relationship.
This is caused by a bad bite (malocclusion) which has two consequences. First, it alters the position of your temporomandibular joints and places excessive pressure on the nerve-filled area surrounding them. Second, it twists, or torques, your jaw into a strained position. This can affect the muscles in your face, head, neck, back and shoulders. Muscles under constant strain are painful!
To correct this, the jaw must be brought back into a muscularly balanced position. Before explaining how this is done, let us discuss how chronic muscle stress affects you emotionally and biochemically.
Diagnosis
MPD is often called "the great imposter." No wonder! Because of the number and variety of symptoms it is difficult to detect. How many people would think of visiting a dentist if suffering from headaches, ear stuffiness, or neck pain? Consequently many go from doctor to doctor trying to find relief. This can be extremely frustrating--and costly! You may even begin to wonder, "am I crazy?" Since MPD is so seldom recognized, people who suffer from it often receive little support.
This is why an accurate diagnosis is so important. It is the key to successful treatment. Below is an outline of a diagnostic procedure. The doctor may use any or all of these procedures to arrive at a diagnosis:
- An interview to discuss your medical history in relation to your MPD condition, onset of pain, symptoms, and contributing factors.
- A clinical examination to explore tenderness in the muscle groups of your jaw, head, neck and shoulders, as well as your teeth and bite, and other related factors such as ear blockage and posture.
- X-rays of your jaw joints in open, closed and rest position.
- Casts (models) of your teeth to obtain a record of your biting and chewing pattern.
- Use of TENS to relax the muscles of your jaw.
- An analysis of your jaw movements.
- An analysis of your muscle activity.
- Recording of jaw joint sounds.
TENS and other instruments that measure jaw movement and muscle activity are widely used in dentistry. We describe these more in our technology page.
Treatment
Once all diagnostic information is collected, we can determine the best course of treatment. Typically, treatment will follow these steps:
- Relieve muscle spasm and pain. TENS is one of the most effective ways to do this. Sometimes moist heat packs applied to the face or muscle massage will also help. Occasionally pain medication or mild muscle relaxant drugs are prescribed.
- Stabilize the bite. When muscles have been tight for a long time, it takes a while for them to relax. During this phase, the bite can be temporarily corrected with the help of a splint, or orthotic, which fits over the teeth. This allows us to make easy adjustments of your bite until it reaches a stable position. Once symptoms are relieved and the bite is stabilized, then it can be permanently built to the correct position.
- Long-term management. There are various ways that your bite can be corrected in a more permanent way. Below are five approaches:
- Coronoplasty/Equilibration -- selectively reshaping the contours of the teeth to correct the bite. This is a fairly simple procedure which can be used when the bite has minor discrepancies.
- Removable Overlay Partials -- permanent orthotics which are designed to maintain an accurate and stable bite.
- Reconstruction -- adding height to the teeth to provide structural support.
- Orthodontics (Braces) -- when teeth are very healthy in both children and adults, they may be moved to the correct neuromuscular position.
- Orthognathic (Jaw) Surgery -- in a very small percentage of cases,surgical realignment of the upper and lower jaws may be required to correct the bite.
What Is An Orthotic?
Orthotics are known by various names, such as splint, or bite guard. The term orthotic is most accurate because it means a mechanical appliance designed for orthopedic use.
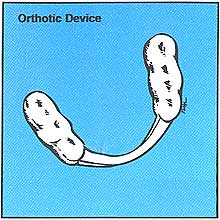
Orthotic Device
Orthotics are also made in various ways. Typically they are made of lightweight clear acrylic and fit over your lower back teeth. Many people who suffer from MPD have back teeth which are too short. The orthotic adds height to your teeth to provide structural support. Providing support for your back teeth rotates your jaw down and forward. With this support, the muscles do not have to strain to bring your teeth together.
What Will the Orthotic Feel Like?
The purpose of the orthotic is to change the way the teeth close together so that the muscles are balanced. It is hard to predict how you will feel at first. Sometimes it takes a while to get accustomed to having something over your teeth.
Eventually, you will become very used to this new position and it will feel strange when your remove the orthotic. Your teeth will feel "lost". They will miss the support. Many patients find that once accustomed to the orthotic, a headache begins shortly after removing it. This usually stops once it is replaced in the mouth. Again, this vividly shows that your teeth must have this extra support in order for the muscles to relax.
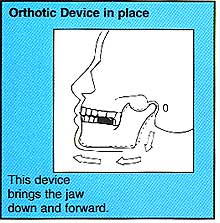
Orthotic Device in Place
Will People Notice That I'm Wearing an Orthotic?
When worn, the orthotic is barely noticeable. The front portion is usually a thin, clear acrylic strip which most people will probably never notice.
How Long Will I Wear an Orthotic?
This is difficult to estimate because each patient is unique. Initially, we must check the orthotic frequently. As your muscles are changing, they may wear or otherwise change the acrylic surface of the orthotic. Gradually, your bite will begin to stabilize and the orthotic will require less frequent checks.
Why Can't I Permanently Wear an Orthotic?
There are several reasons:
- It is usually made of acrylic which does wear down over time.
- Long-term wearing is not hygienic; it can become an irritant to gum tissue.
- It fits tightly around your teeth and over time the orthotic may move them.
Some orthotics have been designed that are appropriate for long term use, and this is something you may wish to discuss with your dentist.
